Computational modeling for drug disposition encompasses the movement and fate of drug molecules within the body after administration, including absorption, distribution, metabolism, and excretion (ADME). Drug distribution specifically refers to how a drug moves from the systemic circulation into various tissues and organs. This understanding is crucial for optimizing drug formulations, determining dosing regimens, and ensuring the safety and efficacy of new drug candidates.
Key Parameters of Drug Distribution The extent of drug distribution is primarily reflected by three parameters:
- Volume of Distribution (Vd): This is a hypothetical volume that represents the relative partitioning of a drug between plasma and tissues. Vd is an important constant that, when combined with drug clearance, can be used to predict a drug’s half-life, which in turn helps determine how often the drug should be administered. Developing computational models for Vd based solely on computed descriptors is still under development due to the scarcity of in vivo data and the complexity of the underlying processes. However, approaches such as Lombardo and colleagues’ model for neutral and basic compounds, using in vitro physicochemical parameters, have shown progress.
- Plasma-Protein Binding (PPB): This parameter describes the extent to which a drug binds to proteins in the plasma. Only the unbound (free) fraction of a drug in plasma is available for distribution into tissues and for pharmacological action. Computational models predict PPB by analyzing molecular structure and electronic configurations, as plasma protein concentration and protein binding nature significantly influence drug distribution. Drugs bind to a variety of plasma proteins, such as serum albumin, α1-acid glycoprotein, and lipoproteins. Acidic drugs tend to bind to albumin, while basic drugs tend to bind to glycoproteins and lipoproteins. Several models have been proposed to predict PPB, with some emphasizing that models should not rely on binding data from only one protein, as PPB is a composite parameter reflecting interactions with multiple proteins.
- Blood-Brain Barrier (BBB) Permeability: This measures a drug’s ability to cross the highly selective BBB, which maintains a restricted extracellular environment in the central nervous system (CNS). For CNS-targeting drugs, crossing the BBB is imperative, while for peripherally targeted drugs, restricting BBB passage is desirable to avoid CNS side effects.
- Modeling BBB Permeation: Most approaches model log blood/brain (logBB), which measures drug partitioning between blood and brain tissue. This is an indirect implication of BBB permeability that does not discriminate between free and plasma protein-bound solutes. More accurate parameters, like log BBB permeability-surface area (logPS), reflect the free drug level in the brain. BBB permeation can be calculated using the polar surface area (PSA) of the molecule and its LogP value, or by passive permeability factor (PS) with LogD (distribution coefficient for an ionized weakly acidic drug at a particular pH). The BBB is composed of endothelial cells, astrocytes, and pericytes, where tight junction (TJ) proteins (e.g., claudin and occludin) play a crucial role in regulating the transport of ions, water, and solutes.
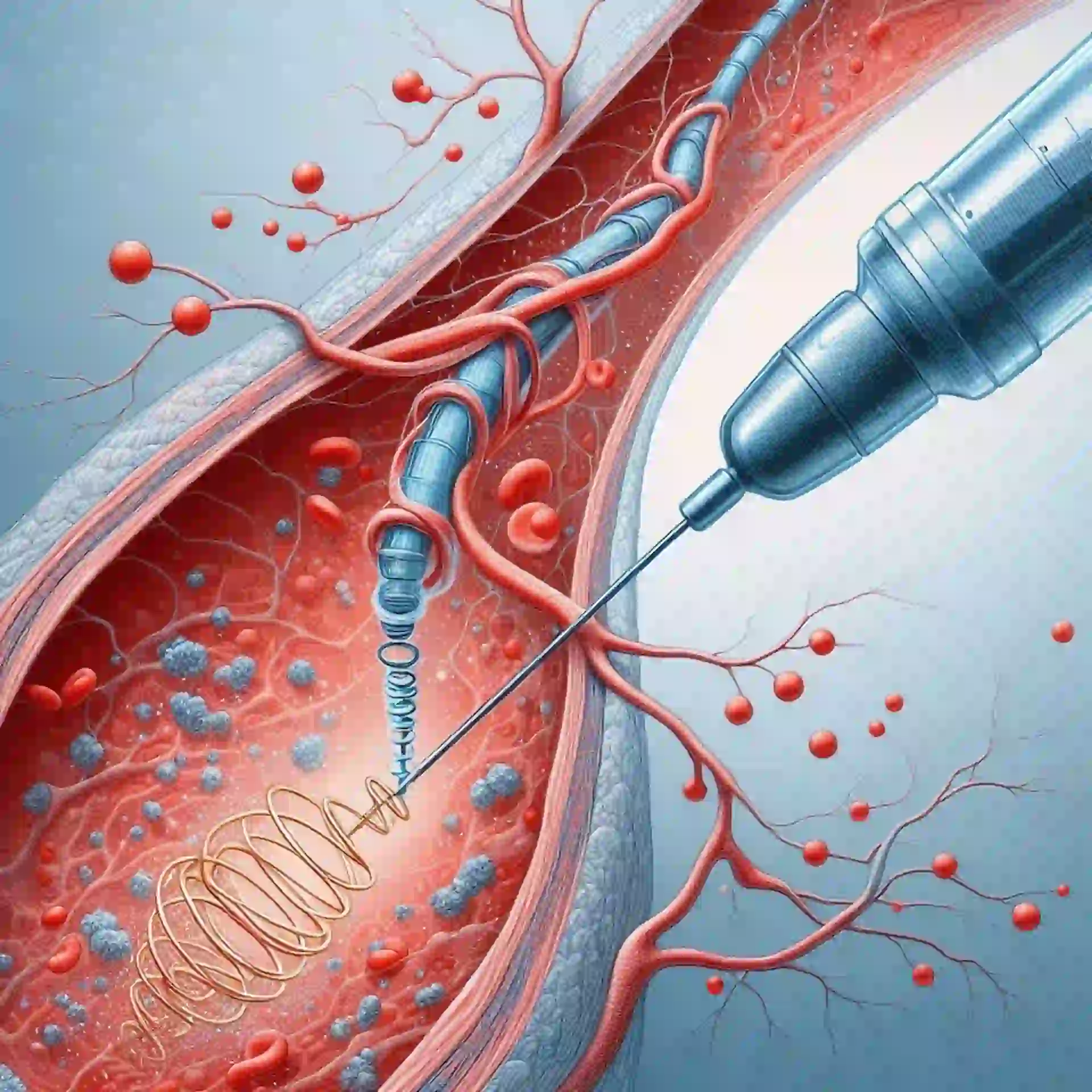
- Role of Active Transporters: The BBB also employs efflux transporters (e.g., P-glycoprotein, BCRP, and BBB-choline transporter) and metabolic enzymes to prevent xenobiotics from entering the CNS. Understanding the structural requirements for transporters like the BBB-choline transporter is crucial for accurate BBB permeation prediction and potential CNS drug delivery.
Computational Modeling Approaches for Distribution Computational models simulate drug distribution by integrating physicochemical, biopharmaceutical, and physiological parameters.
- Physiologically Based Pharmacokinetic (PBPK) Models: These are considered the “gold standard” for simulating drug distribution. PBPK models are mechanistic, multi-compartmental models that represent actual organs and tissues, incorporating physiological parameters such as tissue volumes, blood flow rates, and enzyme/transporter expression. Each compartment in a PBPK model corresponds to a specific organ or tissue. They use mass-balance differential equations to simulate drug distribution, metabolism, and elimination, predicting drug concentrations in plasma and individual tissues over time. PBPK models allow for extrapolation across species, populations, and disease states, and are increasingly used in regulatory submissions. Commercial and open-source PBPK modeling platforms include Simcyp®, GastroPlus™, and PK-Sim.
- Quantitative Structure-Activity/Property Relationship (QSAR/QSPR) Models: These models utilize multivariate analysis to correlate molecular descriptors with ADMET-related properties, including distribution parameters like plasma protein binding. Molecular descriptors can include molecular weight, lipophilicity (LogP), and electronic properties.
- Machine Learning (ML) and Artificial Intelligence (AI) Approaches: ML/AI approaches, including deep learning, random forests, and support vector machines, are increasingly applied to predict complex ADME properties, transporter interactions, and toxicity endpoints using large, heterogeneous datasets. These models can handle high-dimensional data and complex, nonlinear relationships difficult to capture with mechanistic models alone, making them valuable for early-stage screening.
- Molecular Modeling and Simulation: Structure-based methods like molecular docking and molecular dynamics (MD) simulations are used to predict drug-protein interactions, binding affinities, and conformational changes relevant to distribution, particularly for plasma protein binding and transporter interactions at biological barriers.
Factors Influencing Distribution Modeling Beyond the structural and physicochemical properties of a drug, factors such as lipophilicity (often estimated by LogP) and ionization state (determined by pKa and environmental pH) are fundamental inputs for distribution models. Unionized forms are typically more lipophilic and cross membranes easily, while ionized forms generally have higher aqueous solubility. Blood flow and tissue permeability also play significant roles in the extent of distribution.
Unit 2: Computational Modeling of Drug Disposition: Podcast link
Introduction, Modeling Techniques: Drug Absorption, Solubility, Intestinal Permeation, Drug Distribution ,Drug Excretion, Active Transport; P-gp, BCRP, Nucleoside Transporters, hPEPT1, ASBT, OCT, OATP, BBB-Choline Transporter.





